Perspective from HIMSS 2019
Interoperability in healthcare has been a buzzword at HIMSS for over a decade. Recognizing it will take collaboration between providers, payers, and vendors to accomplish this, seven hospital associations recently called for these stakeholders to unite in working to improve the ability to securely share patient information.
As this certainly isn’t a new concept, what has been holding interoperability in healthcare back, and what do we need to overcome to accomplish this goal?
Interoperability in healthcare is the ability for various healthcare information technology (HIT) platforms to exchange, interpret and use data cohesively. The intent of interoperability is to have a holistic view of patients despite the variance in technologies used across practices, hospitals, pharmacies, and other care settings.
![]()
Interoperability in Healthcare:
Ability for healthcare information technology platforms to exchange, interpret and use data cohesively
![]()
Traditional Barriers
Part of what has hindered true interoperability in healthcare is a lack of standardization across these various systems. Original systems used by various departments in the hospital had limited ability to work together, and created siloed systems even within a single facility. Without uniform methods of categorizing or collecting data information, these systems can’t translate each other’s information into meaningful intelligence. Further, current guidelines may discourage the sharing of information as a means to protect patient privacy. Today’s expectation is far more advanced than just data collection, with the need to extract meaning from the data. Therefore, we need information exchange standards that would permit data to be shared across clinician, lab, hospital, pharmacy, and patient regardless of the application or application vendor.
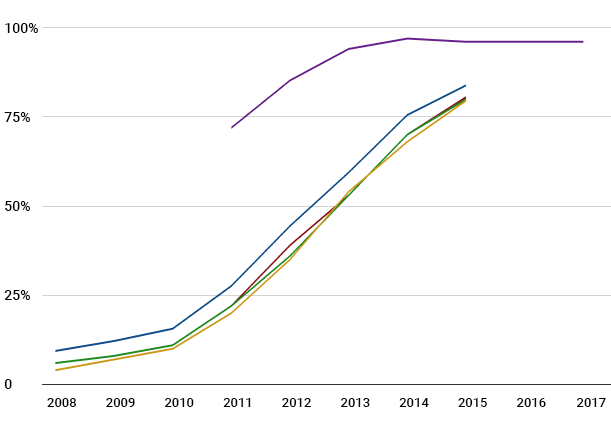
Traditionally, interoperability efforts have also been stilted by uneven adoption of technology across care settings. However, more than 95% of hospitals and nearly 90 percent of office-based physicians have adopted an electronic health record (EHR) system. While work remains to be done to incentivize other care settings including skilled nursing facilities and long term post-acute care centers to adopt similar technology, significant progress has been made in just the last few years.
Providing the Best Care
While patient needs and privacy are of the utmost importance, so is ensuring they are receiving the best care possible. When information is blocked and providers can’t access vital pieces of patient history, is that really in the best interests of the patient? Interoperability means the ability of health information systems to work together within and across organizational boundaries in order to advance the effective delivery of healthcare for individuals and communities.
Just as hospitals last month called for vendors and payers to support information exchange in their systems, as the end-users of these systems, providers are increasingly advocating for change. Many providers and private companies are even launching their own data sharing initiatives, forcing vendor partners to adapt – and vendors that already facilitate the exchange of patient information will come out ahead. Ultimately interoperability facilitates full visibility and access to complete patient data for the healthcare institution, the clinician and the patient increasing quality of care and driving efficiency.
Craig Froude is the Chief Strategy Officer for PipelineRx. A seasoned technology healthcare executive, he is focused on developing new market opportunities, and establishing strategic partnerships and creating product strategies that advance medication management solutions for better patient care.